Miss a day, miss a lot. Subscribe to The Defender's Top News of the Day. It's free.
There was an increase in measles cases reported between 2021 and 2022, according to a Nov. 17 report by the Centers for Disease Control and Prevention (CDC). The report attributed the increase to falling vaccination rates.
U.S. media described the report results as “staggering,” but separate, concurrent CDC data, posted Nov. 2, show only a slight increase in measles cases in the U.S.
According to the CDC’s Morbidity and Mortality Weekly Report (MMWR), global measles cases increased 18% and estimated deaths rose 43% between 2021 and 2022. The number of countries experiencing “large or disruptive” outbreaks also rose between 2021 and 2022, from 22 to 37.
The global decrease in vaccination rates — cited by the CDC as the cause of the increase in measles cases — was small, although the decrease did break a pattern going back more than 20 years.
The data show global measles vaccination rates had been rising steadily, from 72% in 2000 to 86% in 2019. They fell 5 percentage points in 2021, to 81%, but then inched upward again in 2022 to 83%.
The CDC report did not explain how the relatively small changes in vaccine rates could bring about such dramatic increases in measles cases and deaths globally. The authors of the report did not respond to The Defender’s request to explain this.
Estimates cited in report ‘subject to some uncertainty’
The CDC’s percentage increase in global measles cases is based on data provided by 144 reporting countries. However, the agency’s estimate of a 43% increase in fatalities is just that — an estimate, based on previously calculated case fatality rates (CFRs) for specific countries, not death reports.
CFR, which typically measures disease severity, is the percentage of people among all diagnosed individuals who die from a disease during a specified time interval: If 100 people get measles during 2023 and 5 die, the CFR is 5/100 or 5% for that period.
While CFR provides useful information for outbreaks that have already occurred, its predictive value depends on accurate case reporting, health system readiness, the ability to distinguish symptomatic from asymptomatic cases and social factors that may result in case over- or under-estimation.
For example, the general population CFR for COVID-19 was estimated at between 0.4% and 15% early in the pandemic, but official statistics now show the CFR was about 0.9%. The CDC now recognizes that the CFR for COVID-19 was probably much lower still.
Since CFR is not constant but varies depending on the context, time, population, treatment and the patient’s ability to recover, a CFR calculated during one year may not be valid in a subsequent year.
The authors acknowledged these limitations in their report:
“First, vaccination coverage might be affected by data quality issues, leading to inaccurate estimations. Second, the number of specimens submitted for genotyping represents a small proportion of measles cases, so the distribution of genotypes presented might not reflect the global distribution.
“Finally, the output from modeling estimates is dependent on the data input into the model and is thus subject to some uncertainty.”
CDC offers no data supporting claim that vaccination rates are linked to measles outbreaks
Most U.S. media reporting on the CDC global data emphasized the “cases up, vaccinations down” angle.
ABC News headlined the story appropriately — citing the CDC’s numbers on cases and vaccination rates — but reported that “most of the cases were among young people who were not vaccinated, and most outbreaks occur in groups of people who are not up to date on their vaccines.”
However, the CDC did not report the percentage of vaccinated versus unvaccinated infections, or even that infections occurred mainly “among young people who were not vaccinated.”
The CDC report stated only that “failures of routine immunization services to reach children are rapidly revealed by the occurrence of outbreaks primarily affecting unvaccinated children,” but the agency presented no data to support this claim.
Quoting a CDC official, Reuters declared the findings “staggering.” The outlet also reported that interruptions during the COVID-19 pandemic “massively disrupted” worldwide vaccination efforts and recovery has been slow.
The CDC did not use such dramatic descriptions of its findings, but instead let the data speak for itself.
The U.S. was unaffected but authors conclude surveillance and vaccines ‘critical’
The takeaway from the CDC’s MMWR data is that when under stress, developing countries with sub-optimal health systems do worse than developed nations — a variation on the theme that poor people have fewer resources than wealthy people.
Regardless, the CDC’s data show that however “staggering” the rise in worldwide measles rates, the U.S. was unaffected, as shown in Figure 1.
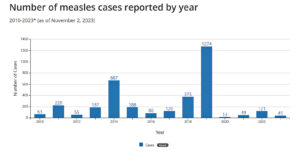
The data in Figure 1, sourced from a separate 2023 CDC report, may be used to make almost any case regarding measles infections and vaccinations.
For example, while 2012-2014 and 2020-2022 are examples of small increases and the 2017-2019 difference may be described as “dramatic,” increases recorded for all three of these time periods occurred while U.S. vaccination rates were rising.
Similarly “dramatic” are the decreases in measles cases between 2014-2016, and between 2019 and any subsequent year, which might be used to support the effectiveness of measles vaccination.
The CDC’s statistical analysis of the data revealed that U.S. case numbers totaling 121 for 2022, the first year following the largest global vaccination drop (5 percentage points), are less than half the U.S. case average — 247 — for the 2010-2023 time period, and almost exactly at the median value for these data, 121.5.
In other words, nothing remarkable.
We also calculated the statistical trend for the 2010-2023 data using an online correlation coefficient calculator. This statistic measures the strength of the relationship between two variables — in this instance, between the year and the number of measles cases.
Since vaccination rates also were rising during the 2010-2023 time period, this relationship also tracks vaccinations to measles outbreaks.
The correlation coefficient is a number between -1 and +1. A value of +1 indicates that a change in the independent variable (year, and by analogy rising vaccination rate) is accompanied by a consistent, predictable increase in the dependent variable (measles cases). A -1 value means cases fall. A value of 0 means no relationship exists.
The correlation coefficient for the data in Figure 1 is -0.000163, which is very close to zero and suggests no relationship between time or vaccination rates and measles cases.
According to the MMWR report, population-based measles immunity requires 95% of children to receive two vaccine doses, an immunization rate achieved by about one-third of the world’s nations.
The authors concluded: “It is critical that all countries and global partners work to accelerate the recovery of vaccination and surveillance programs toward the end goal of regional measles elimination.”
1989 measles outbreak in U.S. raises questions about vaccine efficacy
The U.S. Food and Drug Administration (FDA) approved the first U.S. measles vaccine in 1963 and licensed an improved product, the Edmondson-Enders vaccine, in 1968.
Edmondson-Enders remains the only measles shot distributed in the U.S., but today it is usually combined with immunizations against mumps and rubella (the MMR vaccine) or with protection against mumps, rubella and varicella (MMRV).
Before 1963, nearly everyone got measles by age 15. The CDC estimates that 3-4 million Americans were infected each year, of whom 48,000 were hospitalized, 1,000 developed measles-related encephalitis (brain swelling), and between 400 and 500 died.
Measles cases fell after the initial vaccination campaign and by 1978, the CDC announced its goal of eliminating measles from the U.S. by 1982. Not only was this goal unrealized, but a large 1989 outbreak among vaccinated children prompted experts to recommend a booster MMR dose for all children.
The 1989 outbreak was concerning on several levels. Case numbers totaled 7,335, 380% higher than in 1988. Ten confirmed and 30 suspected deaths also occurred, but 51.2% of those affected were vaccinated.
Among the unvaccinated patients, 18.1% were ineligible for the shot, skewing infection risk toward the vaccinated even more.
The current U.S. vaccination schedule recommends two shots — one between 12-15 months of age, the other between 4-6 years.










