Miss a day, miss a lot. Subscribe to The Defender's Top News of the Day. It's free.
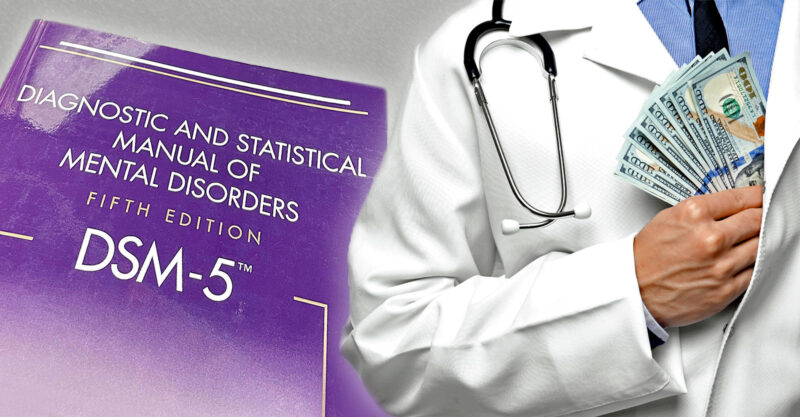
Fifty-five of the U.S. doctors who helped decide what diagnoses and treatments were included in the American Psychiatric Association’s (APA) main diagnostic manual received more than $14 million in undisclosed industry funding, a special report in The BMJ revealed.
According to The BMJ:
“The Diagnostic and Statistical Manual of Mental Disorders published by the American Psychiatric Association standardizes symptom criteria and codifies psychiatric disorders. This manual plays a central role in the approval of new psychiatric drugs and the extension of patent exclusivity, and it can influence payers and mental health professionals who seek third party reimbursements.”
The manual, now in its fifth edition, DSM-5-TR, is often referred to as the “bible” of psychiatric disorders. It was released in 2002 and includes changes made since the APA first published the manual in 2013.
The authors of The BMJ report wrote that “industry influence over the development of this diagnostic guideline can have a profound effect on public health (eg, by broadening diagnostic categories and influencing what drugs will be prescribed and covered by insurance). It is thus critical that authors of this psychiatric taxonomy should be free of industry ties.”
Research consistently shows that conflicts of interest lead to “pro-industry thinking and conclusions,” the authors of the report said.
The BMJ found that the doctors who received the most money — often in the form of food, beverages, travel and consulting reimbursements — were those working in diagnostic areas “where drug interventions are often the standard treatment, such as depressive disorders, neurocognitive disorders, and drug induced movement disorders.”
The study’s lead investigator, Lisa Cosgrove, Ph.D., a professor and clinical psychologist in the Applied Ethics Center at the University of Massachusetts, Boston, told Medscape Medical News, the study’s intent was “not to point fingers at the APA or individual members of the APA but rather to provide hopefully a small piece of research data that would help the APA look at the larger systemic issue of conflicts of interest.”
Justine Tanguay, a lawyer with Children’s Health Defense and research director for the organization’s Reform Pharma initiative, praised the researchers for bringing public awareness to the issue.
Tanguay told The Defender:
“It’s an outrageous concept to think that if a doctor, scientist or public health official is paid or funded by Big Pharma that he or she can present or recommend an independent viewpoint.
“It doesn’t take a rocket scientist to understand that even the perception of a conflict of interest undermines the integrity of medicine.”
The Reform Pharma campaign is working “to systematically remove Big Pharma corruption and to restore the healthcare system” — which is needed now more than ever because “such conflicts of interest … have become the norm,” Tanguay said.
A problem for over a decade
Cosgrove — who previously served as a research fellow at the Edmond J. Safra Center for Ethics, Harvard University — has for over a decade studied conflicts of interest among contributors to the APA’s manual.
The high percentage of doctors with industry ties reported by the latest BMJ study, published Wednesday, mirrors the findings reported in her previous work.
“What we also see that’s consistent with our 2016 study and 2012 study is the panels for which the members had the most financial ties to industry were those for which pharmaceutical interventions are the first line of therapy,” Cosgrove said.
After duplicate names had been removed, The BMJ identified 168 individuals who served as either panel or task force members of the DSM-5-TR. Of those, 92 met the inclusion criteria of being a physician based in the U.S. and therefore could be included in Open Payments, a publicly accessible database.
Eighty-six of the doctors were panel members for the DSM-5-TR. The other six were task force members who also had decision-making powers.
Of these 92 individuals, 55 (60%) received payments from industry. The authors used OpenPayments to look at the funding the 92 doctors received from 2016 to 2019 — the years just before and during the development of the DSM-5-TR.
The amounts ranged from just under $14 per doctor to $2.7 million per doctor. Collectively, the doctors received more than $14.2 million.
Cosgrove and her co-authors found it particularly unethical that more than one-third of the doctors received money as “compensation for services other than consulting, including serving as faculty or as a speaker at a venue other than a continuing education program.”
In other words, these individuals were hired by drug companies as “key opinion leaders” to speak at pro-industry events. Cosgrove and her co-authors said:
“Being on a speakers bureau or being a key opinion leader is widely recognized as an egregious financial conflict of interest because the role of the key opinion leader is essentially a marketing one; the talks given are usually presented at educational events sponsored by industry.”
Dr. Bernard Lo, professor emeritus of medicine and director emeritus of the Program in Medical Ethics at the University of California, San Francisco, agreed. He told Medscape that key opinion leaders are hired by drug companies to give talks, meaning they are used by the industry as “basically salespeople trying to increase sales of a product.
Full public disclosure needed
Before the development of the DSM-5, the APA claimed the organization’s goal was to develop a “transparent process of development for the DSM, and … an unbiased, evidence-based DSM, free from any conflicts of interest.”
An APA spokesperson told Medscape that DSM-5-TR decision-makers were not allowed to participate if the organization was made aware they had received more than $5,000 in industry payments and that all who worked on the text revision were required to disclose all sources of income prior to their participation.
“The APA implemented and enforced a rigorous process for DSM-5-TR that required transparency by all contributors of their personal and professional interests, followed by an independent review to ensure that personal and professional interests did not bias any results,” the spokesperson said.
The study’s findings, however, contradicted that claim by the APA. And the APA did not publicly disclose industry ties for the latest edition of the manual, according to the study authors.
The APA also did not publicly disclose minutes of the DSM meetings, summaries of changes proposed by the panel and task force members or reasons for those changes.
Public disclosure of all industry funding is critical, according to Lo.
“Part of the report should be, ‘Here are the conflicts of interest reported by the members of the panel’ … Failure to do that in the DSM-5-TR is unacceptable from an ethical and transparency point of view,” Lo said.
The APA’s failure to adequately address conflicts of interest doesn’t promote transparency or public trust in the diagnostic criteria published in the DSM-5-TR, he said.
Tanguay agreed. “In order to have trust in medicine, we need to have transparency, whether it covers medical research, scientific publications or public health policy.”
Those with industry ties should be barred
Cosgrove recommended the APA follow the 2011 report, “Clinical Practice Guidelines We Can Trust,” produced by the Institute of Medicine (IOM, now called the National Academy of Medicine). The report is an updated and streamlined version of a 2009 conflicts of interest guideline co-authored by Lo.
“The IOM recommends that the whole guideline development group be free of industry ties,” Cosgrove said. “At a minimum, the chair … and the majority of folks should not have ties to industry.”
Tanguay went further by saying scientists with industry ties should be barred from publication because such ties distort the scientific literature.
Dr. Giovanni A. Fava — a highly regarded researcher and clinician — in 2009 warned, “The increasing influence of the pharmaceutical industry on psychiatric research and practice is leading to an intellectual and clinical crisis.”
While some might argue that banning all those with industry ties would shrink the expert pool that develops the DSM and other guidelines, Cosgrove said that’s not the case.
“There are hundreds of experts in all medical disciplines that do not have industry ties,” she said. “The ‘most experts have industry ties’ is a spurious and unsupported argument.”
The APA should especially ban those who received industry money for serving as key opinion leaders, Lo said.
The APA did not immediately respond to The Defender’s request for comment.