Miss a day, miss a lot. Subscribe to The Defender's Top News of the Day. It's free.
James Lyons-Weiler, Ph.D., recently posed an interesting question to his Substack readers about the Jynneos monkeypox vaccine.
Based on some rough estimates, Lyons-Weiler calculated that the risk of monkeypox after vaccination, based on a study published in the Journal of the American Medical Association (JAMA), is about 50 times greater than in the unvaccinated population of similar at-risk people.
So he asked his readers, “What (respectfully) do you think is going on?”
Lyons-Weiler is (respectfully) pointing out the obvious: If a therapy results in more disease in those who are treated, couldn’t the therapy be causing the disease?
Medpage Today also covered the results of the JAMA study in this article: “Breakthrough Monkeypox Cases Seen Weeks After Second Jynneos Dose,” with the subhead, “However, most post-vaccination cases in at-risk group occurred within 14 days of first dose.”
When so many cases occur — and they occur immediately after the therapy — should these really be called “breakthrough” infections?
The term “breakthrough infection” is a euphemism for “vaccine failure.”
The word “breakthrough” connotes an excusable lapse in protection, an inevitable one-off when a wily and ubiquitous virus manages to penetrate a formidable wall of vaccine-mediated protection.
But is it really a “wall of protection” if the incidence of disease is greater in those who stand behind the wall compared to those who face the attack head on?
In the case of the JAMA study, vaccination wasn’t a “wall of protection” — it was actually a magnet for disease.
We are speaking of vaccine efficacy. If the incidence of disease is greater in the vaccinated, vaccine efficacy is negative — meaning, there is a benefit in avoiding the vaccine.
Results of the Jynneos monkeypox vaccine trial are difficult to swallow for those who accept that all vaccines are “safe and effective” as axiom.
The public has slowly come to accept that the protection of vaccines can “wane,” — but when vaccine effectiveness creeps into negative territory, the vaccines can no longer be considered safe, either.
In that sense, “negative vaccine effectiveness” is also a euphemism. Why don’t we call it what it really is — harm?
COVID vaccine ‘breakthrough’ infections
With regard to COVID-19 vaccine effectiveness against infection, observational data from the U.K. shows an increasing level of harm from inoculation.
As of March 2022, the risk of getting COVID-19 was 2.5 to 5 times higher in people over age 18 (see Table 14 below).
Unfortunately, U.K. health officials unceremoniously announced these statistics would no longer be reported, stating:
“From 1 April 2022, the UK Government will no longer provide free universal COVID-19 testing for the general public in England, as set out in the plan for living with COVID-19.
“Such changes in testing policies affect the ability to robustly monitor COVID-19 cases by vaccination status, therefore, from the week 14 report onwards this section of the report will no longer be published.”
It is unclear how the elimination of free COVID-19 testing will affect the U.K.’s ability to robustly monitor COVID-19 cases by vaccination status.
If anything, it will decrease the amount of indiscriminate testing of asymptomatic individuals — a practice that will (and has) exaggerated the incidence of the disease in everyone tested. One could argue that this change in policy will actually increase the ability to robustly monitor COVID-19 cases.
Nevertheless, here are the last numbers reported by the U.K.:

The first two columns compare rates of infection between fully vaccinated and boosted individuals with the unvaccinated. In every age group over 18, the COVID-19 infection rate is significantly higher.
The authors of this report caution the reader to not jump to any conclusions. They explain:
The case rates in the vaccinated and unvaccinated populations are unadjusted crude rates that do not take into account underlying statistical biases in the data and there are likely to be systematic differences between these 2 population groups. For example:
-
- testing behaviour is likely to be different between people with different vaccination status, resulting in differences in the chances of being identified as a case
- many of those who were at the head of the queue for vaccination are those at higher risk from COVID-19 due to their age, their occupation, their family circumstances or because of underlying health issues
- people who are fully vaccinated and people who are unvaccinated may behave differently, particularly with regard to social interactions and therefore may have differing levels of exposure to COVID-19
- people who have never been vaccinated are more likely to have caught COVID-19 in the weeks or months before the period of the cases covered in the report. This gives them some natural immunity to the virus which may have contributed to a lower case rate in the past few weeks
The first three points are valid concerns when examining two groups of unmatched populations in any observational study. These factors may skew vaccine effectiveness in either direction.
Without any randomized, placebo-controlled, matched cohorts we are left only with large observational data sets like this one from which to draw conclusions. Why wouldn’t they continue to report these numbers if that’s all we can do?
The fourth point is puzzling. The authors suggest that the unvaccinated have “some natural immunity” because they “are more likely to have caught COVID-19” prior to this period of comparison.
Though the authors minimize the protective benefit of natural immunity in their wording, their argument necessitates that natural immunity is superior to vaccination. How else can they use their argument to explain the significantly lower incidence of disease in the unvaccinated?
At the very least, this is a subtle nod to the superiority of natural immunity. However, the authors’ assumption that the unvaccinated were more likely to have caught COVID-19 in “the weeks or months” prior to the period covered in the report flies in the face of their own data.
Were the unvaccinated more likely to have caught COVID-19 prior to this reporting period? No.
Here’s what the previous report showed:

Once again, in every age group over age 18, the case rate in the unvaccinated is less than the rate in the fully vaccinated and boosted. If the unvaccinated are succumbing to COVID-19 less frequently in February, how can they be better protected in March?
According to the authors’ hypothesis, a higher infection rate among the vaccinated in February should have led to a lower infection rate in March. Not only did this not happen, the difference between vaccinated and unvaccinated infection rates were even larger than they were before.
Not only are the vaccinated obtaining a smaller level of future protection from infection compared to the unvaccinated, they are becoming more vulnerable as time passes.
Trend of growing harm
In fact, if we look further back in time we can see that the protective benefit of being unvaccinated is growing month over month. To put it less euphemistically, as time goes on it is becoming clearer that the vaccinated in the U.K. are being harmed.
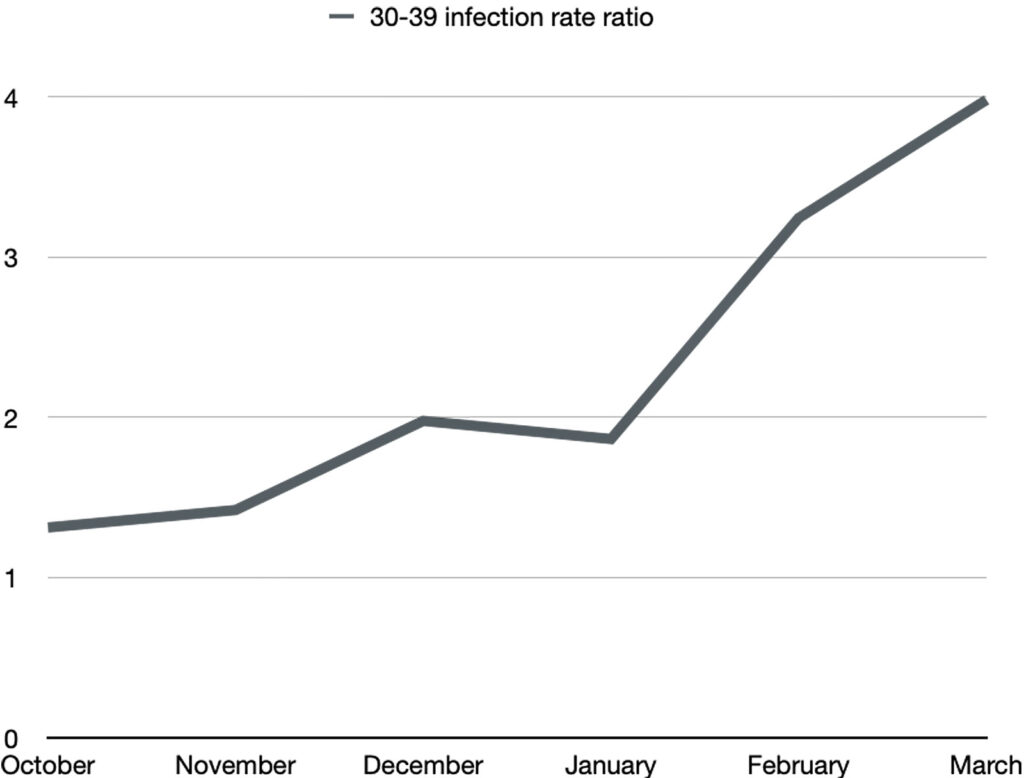
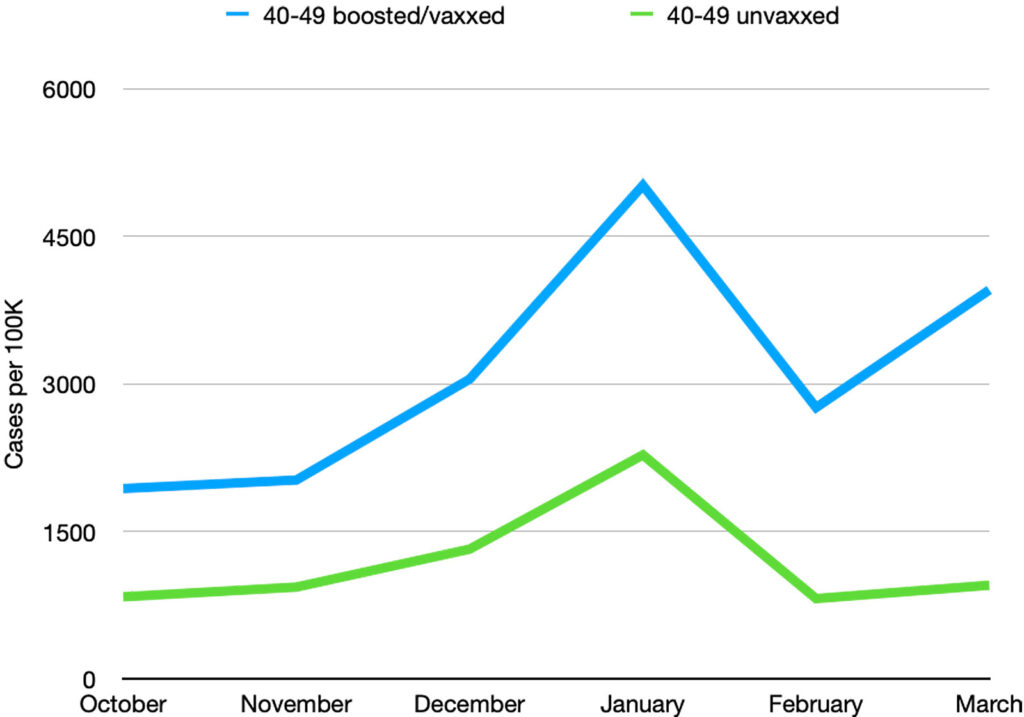
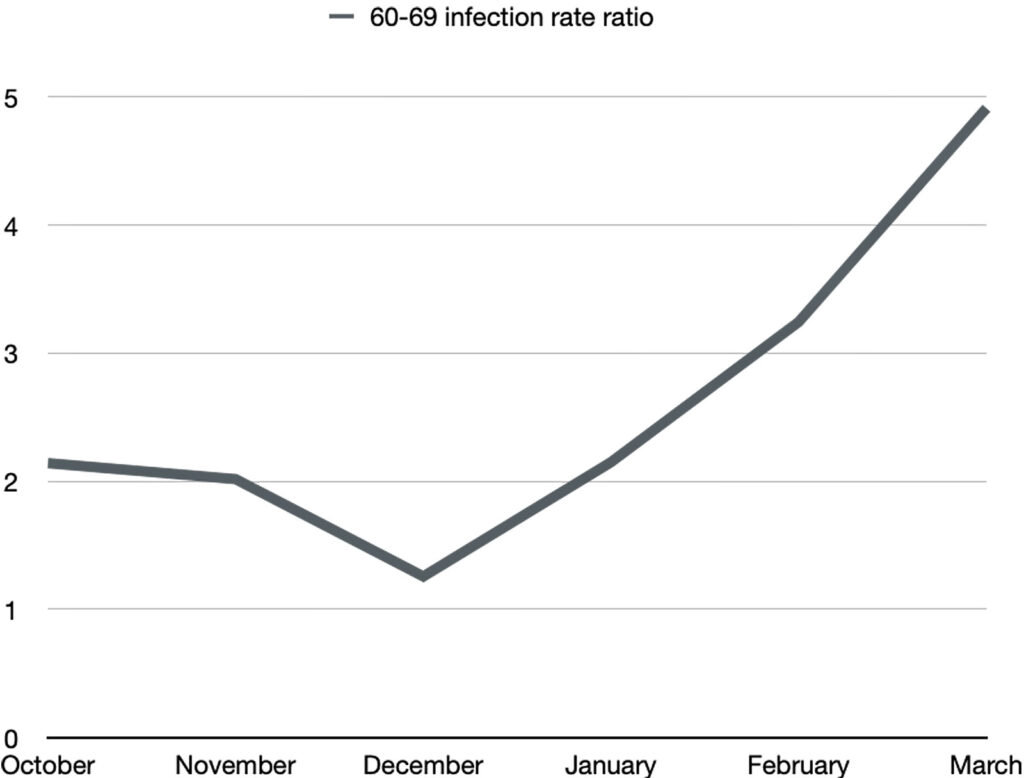
To better illustrate the growing harm, below are the relative infection rates plotted in each age group over the last six months that this data was reported (October 2021-March 2022).
The infection rate in the unvaccinated is in green, and the infection rate in the boosted/vaxxed is in blue.
The ratio of the infection rates is plotted separately in black. A ratio greater than 1 means the infection rate in the boosted/vaxxed is bigger than in the unvaxxed.
Notice that the infection rate in the vaxxed/boosted is not only greater than in the unvaccinated in every age group, but it is increasing with the passage of time. This means that with respect to SARS-CoV-2 infection, the vaccinated/boosted population is doing progressively worse.
Ages 18-29:


Ages 30-39:

Ages 40-49:

Ages 50-59:


Ages 60-69:

Ages 70-79:


Age greater than 80:


In every age category, the COVID-19 infection rate in the boosted is proportionately larger and larger with subsequent months. By March 2022, boosted individuals between the ages of 30 to 79 have approximately a 4 times greater chance of getting COVID-19 than their unvaccinated counterparts.
COVID-19 infection should protect against subsequent infections. However, what we see in the U.K. is that despite having higher infection rates, the vaccinated continue to become infected at even higher rates in subsequent months.
Let’s be clear. The incidence of the disease the vaccine was designed to protect against is several times higher–and growing–in those who got the vaccine. Is the virus “breaking through”? Or is it being encouraged to enter?
Finally, they offer this mystifying caveat in footnote 1 of Table 14:
“Comparing case rates among vaccinated and unvaccinated populations should not be used to estimate vaccine effectiveness against COVID-19 infection.”
Really? How exactly should vaccine effectiveness be estimated? Is there a better way?
Let’s refer to page 4 of the same report, where they explain how it should be done correctly:
“Vaccine effectiveness is estimated by comparing rates of disease in vaccinated individuals to rates in unvaccinated individuals.”
No harm in the U.S.?
Despite the disturbing trends in the U.K., Centers for Disease Control and Prevention (CDC) data continue to demonstrate a benefit with regard to infection rates in the vaccinated.
The most recent data from the U.S. (August 2022) indicates that unvaccinated individuals have a 2.4 times greater risk of contracting COVID-19 than those who are jabbed.
However, CDC data from March 2022 (the period covered in the last U.K. report), show that unvaccinated people under the age of 50 had a lower incidence of disease than those who were fully vaccinated and boosted.
When will the CDC update its datasets? Will the CDC continue to report vaccine effectiveness against infection if it goes negative? Or will it follow the U.K.’s lead and leave us to wonder?
What (respectfully) do you think is going on?